Published: 4 September 2025
Publications
Medicine-induced Pisa syndrome
Published: 4 September 2025
Prescriber Update 46(3): 49–51
September 2025
Medsafe recently reviewed the risk of Pisa syndrome with donepezil (an
anticholinesterase inhibitor) and concluded that there is sufficient
evidence to support an association. We have requested sponsors to update
their donepezil data sheets with this adverse effect. As of 1 August
2025, the New Zealand Pharmacovigilance database has not received any
reports of Pisa syndrome.
What is Pisa syndrome (pleurosthotonus)?
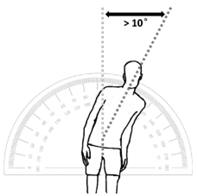
Pisa syndrome (also known as pleurosthotonus) is a rare neurological condition characterised by more than 10 degrees of constant lateral flexion of the spine when the patient is upright (Figure 1). This abnormal posture resembles the Leaning Tower of Pisa, which gives the syndrome its name. Patients may have difficulty with walking or standing up straight. Some patients may be unaware they are leaning.1
There are a variety of causes for Pisa syndrome, and many other conditions can have similar presentations.1 However, Pisa syndrome is most strongly associated with older age, females, neurodegenerative diseases and polypharmacy with antipsychotics and anticholinesterase inhibitors (especially with prolonged use or high doses).1,2
Figure 1: Pisa syndrome – characterised by more than 10 degrees of constant lateral flexion of the spine when upright
Source:
Rissardo JM, Vora NM, Danaf N, et al. 2024. Pisa syndrome secondary to drugs: A scope review. Geriatrics 9(4): 100. DOI: https://doi.org/10.3390/geriatrics9040100 (accessed 27 June 2025).
Medicine-induced Pisa syndrome
A recent review of medicine-induced Pisa syndrome cases reported in the literature found that anticholinesterase inhibitors and antipsychotics were the most frequently reported medicines associated with Pisa syndrome (Table 1).2
The mechanism behind Pisa syndrome is unknown but may be due to an imbalance between dopaminergic and cholinergic neurotransmitters leading to postural control dysfunction.1,2 Medicines associated with Pisa syndrome affect these neurotransmitters.
Table 1: Medicines reported in the literature to be associated with Pisa syndrome (list not exhaustive)
| Medicine class | Medicines |
|---|---|
| Anticholinesterase inhibitors | Donepezil Rivastigmine Galantamine |
| Typical antipsychotics | Haloperidol Chlorpromazine Droperidol |
| Atypical antipsychotics | Quetiapine Risperidone Olanzapine Aripiprazole Clozapine Paliperidone Ziprasidone |
| Antidepressants | Amitriptyline Clomipramine Nortriptyline Mirtazapine Sertraline |
| Antiparkinsonian medicines | Levodopa Pramipexole Ropinirole |
| Mood stabilisers | Lithium |
| Anti-seizure medicines | Valproate |
Adapted from: Rissardo JM, Vora NM, Danaf N, et al. 2024. Pisa syndrome secondary to drugs: A scope review. Geriatrics 9(4): 100. DOI: https://doi.org/10.3390/geriatrics9040100 (accessed 27 June 2025).
Management
Though rare, Pisa syndrome is a recognisable and often reversible condition.2 However, the time between starting the medicine and the onset of symptoms is unpredictable, and it may occur weeks to months later.1
Consider medicines as a possible cause of new-onset postural abnormalities consistent with Pisa syndrome. Symptoms usually resolve after stopping the medicine or reducing the dose.1
References
- Rissardo JM, Vora NM, Danaf N, et al. 2024. Pisa syndrome secondary to drugs: A scope review. Geriatrics 9(4): 100. DOI: https://doi.org/10.3390/geriatrics9040100 (accessed 27 June 2025).
- Lee Y-F. 2018. Antipsychotic-induced Pisa syndrome. Clinical Neuropharmacology, 41(2): 60–3. DOI: https://doi.org/10.1097/wnf.0000000000000274 (acessed 27 June 2025).





